Colposcopy Explained: What It Is, Why It Matters, and How to Prepare
When your Pap smear comes back abnormal, the word “colposcopy” can send a chill down your spine. In reality, it’s not a scary procedure but a powerful tool that gives you a clear window into your cervical health. This guide demystifies colposcopy, explains why it’s often recommended, walks you through the steps, and answers the most common questions.
What Is a Colposcopy?
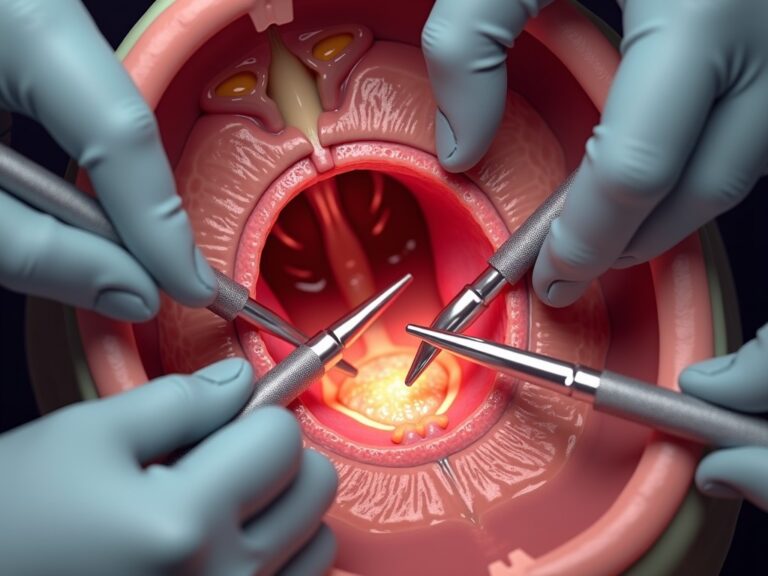
A colposcopy is a specialized examination of the cervix, vagina, and vulva using a colposcope—a handheld microscope that magnifies the area up to 40 times. Unlike a routine pelvic exam, the colposcope provides a detailed, illuminated view that allows the clinician to spot tiny cellular changes invisible to the naked eye.
Key Features of the Colposcope
- High‑magnification (10–40×) for precise visualization
- Bright, focused light that highlights tissue texture and vascular patterns
- Non‑invasive: the device sits outside the body, only illuminating the surface
Why Is a Colposcopy Often Ordered?
Colposcopy is typically recommended after an abnormal Pap smear, a positive high‑risk HPV test, or when a clinician notices suspicious lesions during a routine exam. It’s a proactive step, not a diagnosis of cancer.
Common Triggers for a Colposcopy
- Abnormal Pap Smear Results: Findings such as ASC‑US, LSIL, or HSIL prompt closer inspection.
- High‑Risk HPV Detection: Certain HPV types are linked to cervical cell changes.
- Visible Lesions: Any suspicious area seen during a pelvic exam.
- Unexplained Post‑coital Bleeding: To rule out underlying pathology.
What to Expect During the Procedure
The colposcopy itself is quick—usually 10 to 15 minutes—and takes place in a standard gynecological exam room.
Step‑by‑Step Overview
- Preparation: You’ll lie on the exam table, and a speculum will be inserted to expose the cervix.
- Inspection: The colposcope is positioned outside the vagina, illuminating and magnifying the cervix.
- Application of Solutions:
- Acrylic Acid (Acetic Acid): Turns abnormal cells white, creating a contrast.
- Lugol’s Iodine: Healthy cells turn brown; abnormal cells remain pale or yellow.
- Biopsy (if needed): If suspicious tissue is identified, a small sample is taken for pathology.
What It Feels Like
Most patients report a mild, brief sensation of pressure or a slight sting when solutions are applied. A biopsy may cause a cramp‑like feeling similar to menstrual cramps, but it’s generally well tolerated.
Interpreting Your Results
After the procedure, your clinician will discuss the findings. If a biopsy was performed, results typically arrive within a few weeks.
Possible Outcomes
- Normal: No abnormal cells detected.
- CIN 1 (Low‑Grade Squamous Intraepithelial Lesion): Mild changes; often resolves spontaneously.
- CIN 2/3 (High‑Grade Lesions): More severe changes that usually require treatment such as LEEP or conization.
- Cervical Cancer: Rare, but early detection allows for effective treatment.
After the Colposcopy: Care and Follow‑Up
Immediately after the exam, you may notice light spotting or a brown discharge. It’s normal to avoid sexual intercourse, tampon use, and swimming for a few days. Your provider will give specific instructions based on your findings.
Frequently Asked Questions
Is a colposcopy painful?
Most patients experience only mild discomfort. The procedure is brief, and any sensations are usually short‑lived.
Do I need to fast or take medication before a colposcopy?
No special preparation is required. Just wear comfortable clothing and bring any relevant medical records.
Will a colposcopy replace future Pap smears?
No. Colposcopy is an investigative tool. Routine Pap smears and HPV testing remain essential for ongoing cervical screening.
What if the colposcopy shows no abnormalities?
That’s a good sign. Your provider may recommend routine follow‑up or repeat screening in the usual interval.
Conclusion
A colposcopy is a routine, low‑risk procedure that plays a crucial role in early detection and prevention of cervical cancer. Rather than a cause for alarm, it’s a proactive step toward safeguarding your health. If your doctor recommends a colposcopy, view it as an opportunity to gain clarity and peace of mind about your cervical well‑being.
Remember: an abnormal Pap smear does not automatically mean cancer. With timely colposcopy and appropriate follow‑up, most cervical abnormalities can be managed effectively and with minimal impact on your life.